Free Cancer Screening Guidelines
Lung Cancer Awareness Month: Wildfires and Cancer
It’s already November and the dystopian year of 2020 has hardly been mundane. The year began with Australia ablaze, sending the world into a panic about the wellbeing of Australians and their notorious animals. As the year continued, health and wellbeing remained a priority for people around the world. Now,…...
Small Cell Lung Cancer vs. Non-small Cell Lung Cancer: What’s the Difference?
From a distance, lung cancer may seem straightforward and cut-and-dried. The name itself sparks an immediate mental image of the balloon-like organ located in the chest cavity. It’s common knowledge that tobacco smoke is the leading cause of lung cancer, and that it is amongst the most common type of…...
Why is Lung Cancer So Deadly?
Only 16% of lung cancers are identified at an early stage, making treatment and survival much more difficult. Each year, hundreds of thousands of Americans are diagnosed with lung cancer. Tragically, lung cancer is amongst the deadliest form of cancer, claiming more lives each year than breast, prostate, and colon…...
Targeted Lung Cancer Therapy
A Match Made Possible A discovery by a team led by Massachusetts General Hospital’s Daniel Haber, M.D., Ph.D., a physician-scientist supported by the National Foundation for Cancer Research since 2003, now represents a source of hope for many patients with metastatic lung cancer. He and his colleagues correctly linked very…...
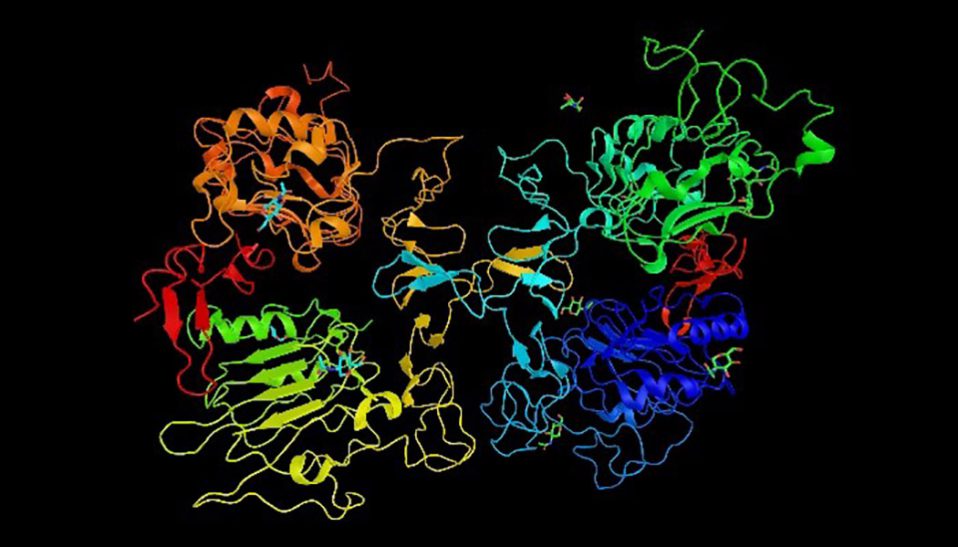
New Type of Lung Cancer Identified
A research team at Cold Spring Harbor Laboratory discovered a new kind of small-cell lung cancer (SCLC). While the general public may not consider this particularly good news, the identification paves the way for developing more specific and personalized medicine approaches to target this previously unnoticed form of the disease....
Lung Cancers Can Differ by Race
According to Clinical Cancer Research, a journal of the American Association for Cancer Research, recently discovered genetic differences in non-small cell lung cancers (NSCLCs) between some African-Americans and European-Americans suggest that there are racial differences in the biology of the disease. These findings could have a clinical impact on personalized…...
- 1
- 2