Free Cancer Screening Guidelines
Detecting Skin Cancer with Artificial Intelligence and Other Game-Changing Technologies in Cancer
Cases of skin cancer are skyrocketing. In the past three decades, more people have been diagnosed with some form of skin cancer than all other cancers combined. Because of this, researchers worldwide have been fascinated with figuring out how to better detect and treat skin cancer. The fascination has launched…...
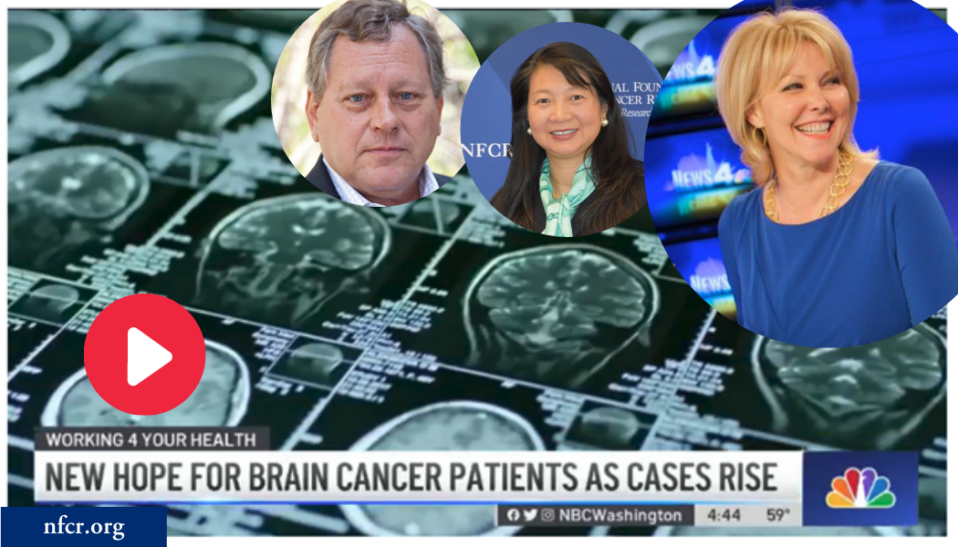
The World’s First Oncolytic Virus Drug was Launched to Treat Malignant Brain Tumor GBM
Glioblastoma multiforme (GBM) is the most aggressive malignant brain tumor in adults, with a median survival of only about ten months. Unlike low-grade gliomas (grades I and II), which grow slowly, high-grade gliomas (grades III and IV) grow much faster and can spread to other parts of the brain, resulting…...
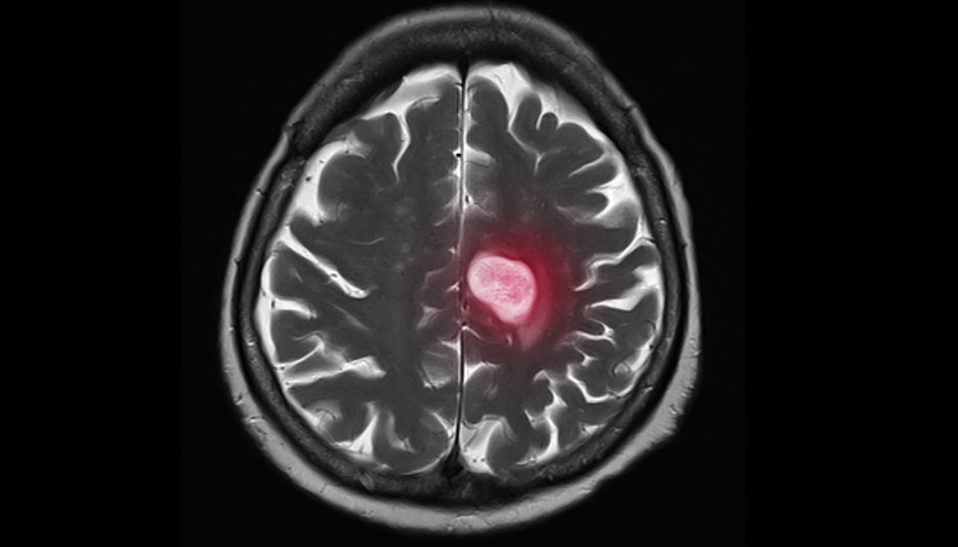
New Brain Scan Technology Can Improve Tumor Removal
Any illness or disease that impacts the brain is highly complex. None more so than brain tumors, which affect over 20,000 Americans each year. While surgeons have become more advanced in the removal of brain tumors, experts continue to face extreme challenges in ensuring all cancerous tissues are removed during surgery. That…...