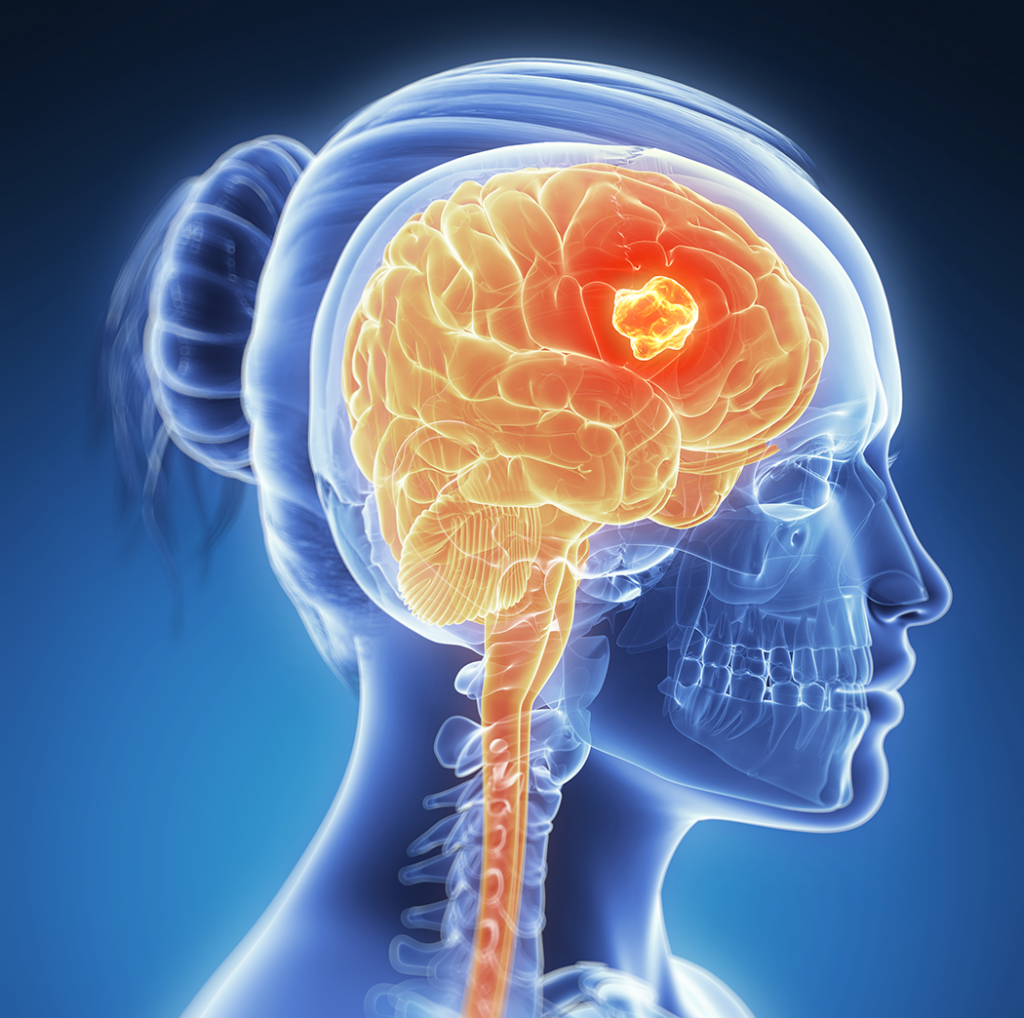
Brain Cancer Awareness Month
In recognition of Brian Cancer Awareness Month, the National Foundation for Cancer Research today offers up a rather in depth overview of a handful of innovative technologies being explored in labs to address the terrible disease class.
Although brain cancer only makes up 1.4% of all new cancer cases, the reality of the lasting and life-altering cognitive, physical and psychological compromises from brain cancer make it particularly scary. Even benign tumors can cause significant changes in people’s lives, depending on what brain regions are being affected. Not to mention that no brain regions are off limits for tumor progression, and many regions are hard to directly biopsy and/or monitor during treatment. That is to say that all areas of the brain are subject to any of the 130 different brain tumors types.
This variability in presentation, along with the difficulty of tracking, is part of what makes brain cancer treatment challenging. As the 10th deadliest cancer in the U.S., the brain cancer mortality rate is 25.5% for people ages 65-74. This is partially a result of that fact that only five drugs are approved for brain tumors, despite the 78 investigational drugs that have been researched in the last 20 years. Furthermore, the brain cancer mortality rate is not dropping at the same speed as other cancers.
It is clearly time to raise awareness of and spending towards brain cancer research, detection and treatment.
Understanding the risk factors for any disease can help provide guidance on how to reduce incidences. Unfortunately, there isn’t a lot of conclusive research towards environmental risk factors for brain cancer. The only clear environmental hazard is exposure to ionizing radiation. The other conclusive risk factor is familial history, although this correlation is not strong—only about 5%. On the other hand, there are anti-cancer behaviors that do help prevent brain cancers. Included are dietary factors such as high fruit and vegetable consumption by the mother during pregnancy and the child in early years of life. In addition, having chicken pox and having adult allergies have been shown to reduce brain cancer risk.
There are some new and potentially exciting advancements in brain cancer treatment. Extracellular vesicles (EVs) are one of these potentially potent new technologies. Extracellular vesicles are tiny lipid particles that can carry molecules through the bloodstream in order to monitor a tumor’s composition and response to therapy.
Although not a cancer drug, this technology may allow for much more elegant and precise brain cancer treatment. It can do so by providing useful information on how a cancer is responding to various treatments in real time. This technology is particularly interesting for brain cancers which are hard to biopsy, and has already shown success in gaining information about the condition of glioblastoma multiforme (GBM), a particularly deadly type.
Shannon Stott, Ph.D., of the Massachusetts General Hospital Cancer Center and the BioMEMS Resource Center, who was instrumental in developing this technology, says that EVs were designed to be a low-cost, easy to use devices that could likely be brought into clinical practice swiftly.
“We are excited by… early-stage data, and look forward to scaling the technology and increasing the number of patient samples analyzed,” Dr. Stott notes. “Specifically, we are interested in exploring how these vesicles change over time in response to treatment, and we see our blood-based assay as an ideal way to explore this in brain tumor patients.”
Tumor vaccines, angiogenesis inhibitors and growth-factor inhibitors are all also being investigated and used for brain cancers. All of these new treatments are focused on reducing cancer development and metastasis by minimizing the factors which promote tumor growth. These factors include both the protein growth-factors and proteins which allow cancer cells to escape white blood cell notice.
Growth-factors have been consistently shown to be essential attributes of tumors. Their suppression minimizes the tumors’ ability to condition its internal and external environment for growth. Tumor vaccines, on the other hand, can help assist in the recognition of tumors by the patient’s own immune system. With optimal recognition, the immune system can treat the cancer as a foreign entity which it organizes around to destroy. While anti-angiogenesis drugs prevent the growth of blood networks which feed the tumor. All of these approaches have worked successfully for other cancers. With more research and fine-tuning of these drugs, it is hoped that they will work for brain cancer as well.
The National Foundation for Cancer Research continues to support scientists performing cutting edge work in many of the areas outlined above, especially angiogenesis and growth-factor treatment efforts for brain cancer. For example:
- NFCR support from 1980 to 2016 for Harold Dvorak, M.D., facilitated his pioneering discovery in 1986 of vascular endothelial growth factor (VEGF), providing the molecular basis for the field of angiogenesis. This discovery led the research community to develop VEGF inhibitors that increase survivorship in five types of cancers but are without benefit for GBM.
- Instead of the accepted mechanism of shutting down blood vessel growth, discoveries by NFCR-supported scientist, Rakesh Jain, Ph.D., on how anti-VEGF drugs work led to a paradigm-shift in the angiogenesis field. He and his team showed anti-VEGF therapy transiently “normalizes” GBM tumor vessels, allowing for a window of opportunity associated with increased blood flows making radiation therapy more effective. Dr. Jain’s team current research has promising results for a new therapeutic approach for GBM which combines treatment types.
- Former NFCR-supported scientist, Web Cavenee, Ph.D., now chairman of our organization’s Scientific Advisory Board, uncovered a mutant version of the Epidermal Growth Factor Receptor (EGFR) – named EGFRviii – most frequently found in GBM tumors. He has led a team to develop monoclonal antibodies to target EGFRviiii and a version is now in clinical trials.
Sign-up to receive related articles directly in your inbox:
References:
- http://www.abta.org/brain-tumor-information/risk-factors/
- http://braintumor.org/brain-tumor-information/brain-tumor-facts
- https://www.cancer.net/cancer-types/brain-tumor/risk-factors
- https://www.cancer.org/cancer/brain-spinal-cord-tumors-adults/about/new-research.html
- https://www.curetoday.com/community/jeannine-walston/2017/05/10-essential-facts-about-brain-tumor-awareness-month-from-a-19-year-survivor
- https://www.ncbi.nlm.nih.gov/pubmed/6318976
- https://www.sciencedaily.com/releases/2018/02/180227155856.htm