Brain Cancer
People of all ages are diagnosed with brain cancer, but there is more frequency among children and older adults. Brain cancer is the second most commonly diagnosed cancer in children (after leukemia).
Key Facts
- Estimates of 94,390 brain tumors will be diagnosed in the U.S. this year, and approximately 28% will be considered malignant – or cancerous.
- An estimated 24,810 malignant tumors of the brain and spinal cord will be diagnosed in the U.S. in 2023, with around 18,990 deaths expected to result from the diagnosis.
- Overall, the chance that a person will develop a malignant tumor of the brain or spinal cord in his or her lifetime is less than 1% (about 1 in 143 for men and 1 in 185 for women).
- Survival rates vary widely depending on the type of tumor.
- Glioblastoma (GBM) is the deadliest type of brain cancer, accounting for 45% of all malignant brain tumors and the five-year average survival rate is only 5% or less.
Source: American Cancer Society’s Cancer Facts & Figures 2023 and American Brain Tumor Association’s Brain Tumor Statistics; Global Coalition for Adaptive Research
Signs and Symptoms
A symptom is a change in the body that a person can see and/or feel. A sign is a change that the doctor sees during an examination or on a laboratory test result. If you have any of the symptoms below, it does not mean you have cancer but you should see your doctor or health care professional so that the cause can be found and treated, if needed.
- Headaches
- Seizures
- Difficulty thinking and/or speaking
- Changes in personality
- Loss of balance
- Change in vision including blurriness, double vision, abnormal eye movements, light sensitivity and loss of vision
- Memory loss
- Disorientation
- Fatigue and muscle weakness
- Muscle weakness
- Depression
- Anxiety
- Tingling or stiffness on one side of the body
Source: National Brain Tumor Society 2023


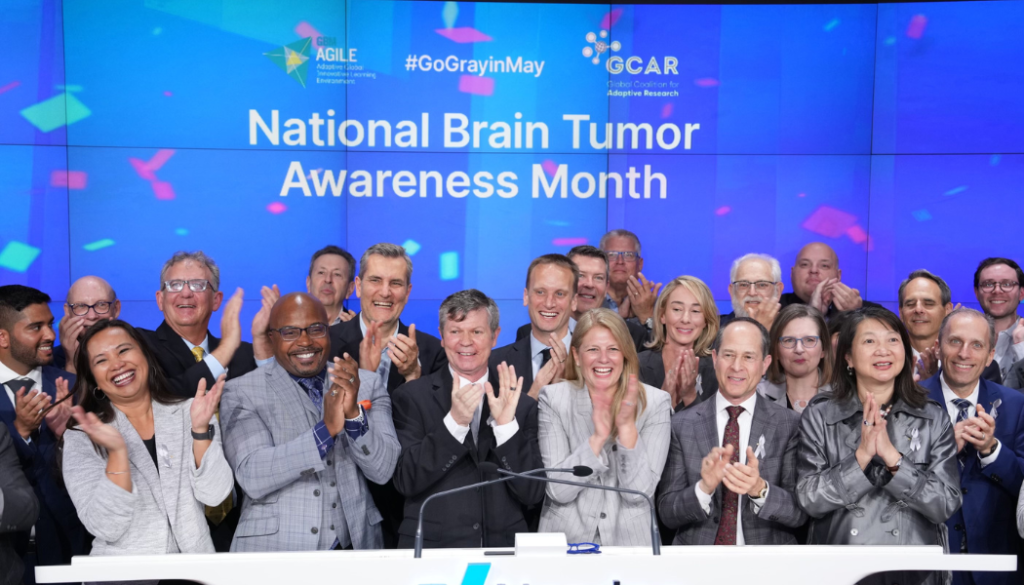
Brain Cancer Awareness Month is recognized in May. To help accelerate cures please make a gift today.