NFCR-Supported Researcher Leads Study Aiming to Understand Which Patients May Respond Best to Immunotherapy
New approach developed by Dr. Rakesh Jain and his research team identifies biomarkers that may indicate which patients will best respond to immune checkpoint blockade therapies.
A research team led by NFCR-supported scientist Rakesh K. Jain, PhD, the Andrew Werk Cook Professor of Tumor Biology at Harvard Medical School and director of the Edwin L. Steele Laboratory for Tumor Biology at Massachusetts General Hospital, made headlines in September with a new study in the Proceedings of the National Academy of Sciences (PNAS) that details the novel approach team members developed to help identify potential biomarkers that may indicate which patients will best respond to immune checkpoint blockade-based therapies.
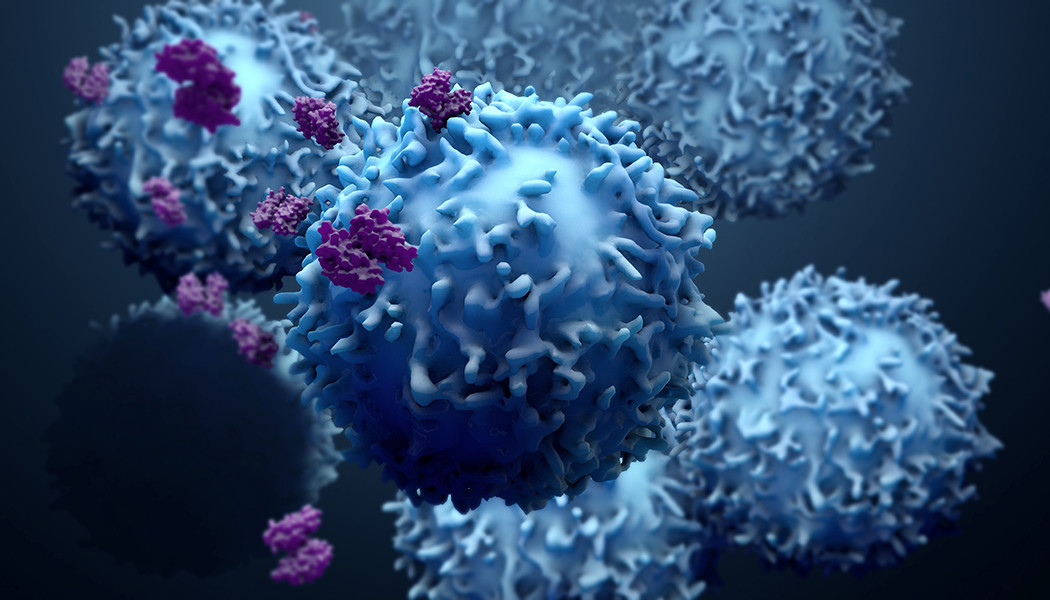
Immune checkpoint blockade (ICB) has revolutionized how doctors treat many types of cancer, with several monoclonal antibody therapies — a type of ICB — now approved by the U.S. Food and Drug Administration to treat more than 20 cancers.1 However, although these therapies are incredibly successful when they work, they are not effective for many patients.
In their study, Dr. Jain and his team sought to identify biomarkers that could not only measure the effectiveness of ICB before and/or shortly after treatment has started, but also help other researchers understand the underlying mechanism(s) that contributes to a patient’s response or resistance to the treatment. The team used a model of bilateral tumor implantations — implanting tumor cells in each side of mouse breast — followed by resection and immunotherapy-response assessment to study the tumor microenvironment shortly after treatment, allowing them to identify biomarkers for response or resistance early in treatment.1 Using this novel approach, the research team found that the tumors that responded to the ICB-based therapy contained higher numbers of cancer-killing T immune cells and fewer numbers of certain immune suppressor cells after treatment was initiated.2
Further analyses also showed that the T immune cells found within the tumors had unique gene signatures that allowed researchers to differentiate between responders and non-responders.2
While this study focused on breast cancer tumors, Dr. Jain and his team are confident that their model could be applied to other cancers to help researchers identify response and resistance biomarkers for ICB-based therapy and guide the use of combination therapy to further boost the efficacy of these therapies.1
To read the full study publication, please visit the PNAS website.
About Dr. Jain:
A world-renowned expert in understanding how changes in the tumor microenvironment affect the immune system, drug delivery, treatment efficacy, and patient survival, Dr. Jain has received funding from NFCR for more than 20 years. Most recently, his NFCR-supported work has focused on understanding why immune checkpoint inhibitors do not appear to be effective in the treatment of glioblastoma — an incredibly aggressive brain tumor. Studies conducted by Dr. Jain and his research team have found that the resistance of glioblastoma to treatment with immune checkpoint inhibitors is due, in part, to the tumor environment, noting that the abnormal vessels found in this tumor severely limit the ability of the immune system’s cancer-killing T immune cells to enter and destroy tumor cells.
To learn more about Dr. Jain’s NFCR-supported research, please visit his webpage.
About Immunotherapy:
Immunotherapy uses the body’s own immune system to fight infections and diseases, including cancer. Treatments focus on helping the immune system better recognize cancer cells, as well as strengthening its response to destroy them. There are currently five different types of immunotherapies available to treat certain types of cancers: checkpoint inhibitors, T-cell transfer therapy, monoclonal antibodies, cancer vaccines, and immune system modulators. Although immunotherapy does not work for every patient diagnosed with cancer, it can be an incredibly successful treatment option for some patients with certain cancers.
To learn more about immunotherapy and its benefits for patients diagnosed with cancer, check out our blog post titled, “Immunotherapy: Fighting Cancer and More?”
Additional Reads You May Enjoy:
GBM AGILE – Changing the Way We Fight Brain Cancer
New Discovery May Significantly Broaden the Applicability of T-Cell Immunotherapy
Stay connected with us! Receive our monthly e-newsletter and blogs featuring stories of inspiration, support resources, cancer prevention tips and more. Sign up here.
___________________________________________________________________________________
References:
1 Ivy X. Chen, Kathleen Newcomer, Kristen E. Pauken, Vikram R. Juneja, Kamila Naxerova, Michelle W. Wu, Matthias Pinter, Debattama R. Sen, Meromit Singer, Arlene H. Sharpe, Rakesh K. Jain. A bilateral tumor model identifies transcriptional programs associated with patient response to immune checkpoint blockade. Proceedings of the National Academy of Sciences. Sept. 2020, 117 (38) 23684-23694; DOI:10.1073/pnas.2002806117
2 Markers may predict patient response to immune therapy of cancer (2020, September 7). Retrieved 14 November 2020 from https://medicalxpress.com/news/2020-09-markers-patient-response-immune-therapy.html