Credentials
Massachusetts General Hospital Cancer Center
Harvard Medical School
Boston, Massachusetts
Assistant Professor of Medicine, Harvard
Co-leader of the Computational Support Group, MGH Cancer Center
Research Projects
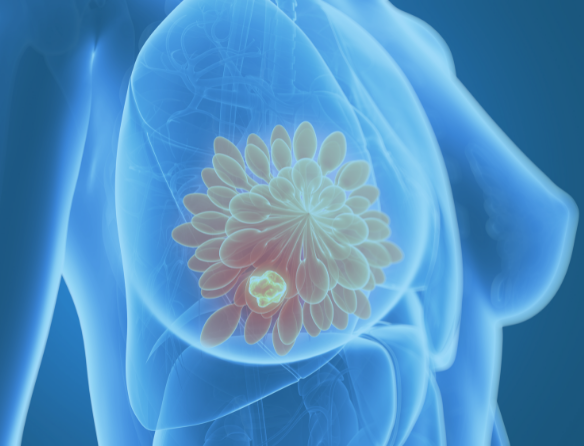
Dr. Rheinbay and NFCR-supported scientist, Dr. Daniel Haber, are collaborating to identify therapeutic targets that may lead to novel therapies for the most deadly subtype of breast cancer, triple negative breast cancer (TNBC). As many as 10% of TNBC exhibits overexpression or amplification of the Androgen Receptor (AR). However, unlike prostate cancer, AR expression in TNBC does not correlate with response to anti-androgens. They will determine whether this pathway can lead to a new treatment option in TNBC.
From circulating tumor cells (CTCs) from patients with and without amplification of the AR, sequencing data will be collected and from experiments that deplete the AR and its co-factor, FoxA1. Dr. Rheinbay will computationally analyze the sequencing and omic (genomic and transcriptome) data. Analysis of the data will identify genes that are differentially altered. Her lab will track genomic changes to identify potential transcription factors and DNA regulators that bind to the gene areas (loci) and contribute to the changes. This may lead to identification of downstream targets for further exploration of enriched molecular pathways.
Background
Dr. Esther Rheinbay is an Assistant Professor of Medicine at Harvard Medical School, a Principal Investigator and the co-leader of the computational Support Group at Massachusetts General Hospital Cancer Center.
Dr. Rheinbay received her Ph.D. Bioinformatics from Boston University in 2012 and completed post-doctoral studies at MGH and the Broad Institute at MGH in 2018 prior to joining the faculty at Harvard in 2019.
Dr. Esther Rheinbay’s research is focused on the identification and characterization of non-coding somatic mutations in cancer, in particular those occurring in gene promoter regions. Her group has a specific focus on studying breast cancer genomics and epigenomics and the FOXA1 breast cancer oncogene.

Our approach emphasizes a collaborative, team environment to accelerate new breakthroughs.