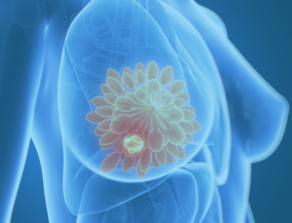
Breast Cancer
About Breast Cancer
Breast cancer is the most common cancer in women worldwide, claiming the lives of hundreds of thousands of women each year. Although it’s rare, men can also be diagnosed with breast cancer. With breast cancer continuing to impact so many people, it’s important to understand the disease and what strides researchers are making.
Breast Cancer Key Facts
- An estimated 313,510 new cases of breast cancer will be diagnosed in the U.S. in 2024, and an estimated 42,780 deaths will occur.
- More than 4 million breast cancer survivors live in the U.S. today.
- The lifetime risk of getting breast cancer in the U.S. is about 1 in 8 for women and 1 in 726 for men.
- Research shows only 5-10% of breast cancers are hereditary.
- Dense breasts can be 1.5 to 2 times more likely to develop cancer. If you have dense breasts, ask your doctor about extra screening tests, like ultrasound or MRI, to check for tumors that a mammography might have missed.
- Triple-negative breast cancer differs from other types of invasive breast cancer as they grow and spread faster, have limited treatment options, and have a worse prognosis (outcome).
- A lump isn’t the only sign of breast cancer. Call your doctor if you notice any of the changes shown below.
Source: American Cancer Society’s Cancer Facts & Figures 2024
For ALL Women:
- Keep a healthy weight
- Be physically active
- Avoid or limit alcohol
- Be cautious of taking hormones
- Breastfeed
- Annual mammograms
For Women at Increased Risk:
- Genetic testing and counseling
- Close observation
- More frequent doctor visits for breast exams
- Starting breast cancer screening with mammograms at a young age
- May adding another screening test, such as an MRI
- Medicines to lower breast cancer risk
- Prevention surgery
- Women with very high breast cancer risk: Bilateral Prophylactic Mastectomy
- Women already diagnosed with breast cancer: Contralateral Prophylactic Mastectomy
- Women with BRCA1 or BRCA2 mutation have a high risk of developing breast cancer and ovarian cancer: Prophylactic Oophorectomy (removal of the ovaries)
Resource:
What Can I Do to Reduce My Risk of Breast Cancer? | CDC
Can I Lower My Risk of Breast Cancer? | American Cancer Society
- Swelling of all or part of a breast (even if no lump is felt)
- Skin dimpling (sometimes looking like an orange peel)
- Breast or nipple pain
- Nipple retraction (turning inward)
- Nipple or breast skin that is red, dry, flaking or thickened
- Nipple discharge (other than breast milk)
- Swollen lymph nodes (Sometimes breast cancer can spread to lymph nodes under the arm or around the collar bone and cause a lump or swelling there, even before the original tumor in the breast is large enough to be felt.)
- New lump or mass on the breast (can be painless, tender, soft, or round)
Source: American Cancer Society 2024
Risk Factors You Cannot Change:
- Getting older – risker when you get older, most found in women age 55 and older
- Genetic mutations
- Sex – much more common in women
- Race/Ethnicity
- Being taller
- Reproductive history
- Having dense breasts
- Having certain benign breast conditions
- Personal history of breast cancer or certain non-cancerous breast diseases
- Family history of breast or ovarian cancer
- Previous treatment using radiation therapy
- Exposure to the drug diethylstilbestrol (DES)
- Starting menstrual periods early
- Going through menopause later
- Having radiation to your chest
Lifestyle Related Risk Factors:
- Alcohol Use
- Not being physically active
- Obesity
- Not having children or first pregnancy after 30
- Not breastfeeding
- Birth Control
- Menopausal hormone therapy
- Breast implants (rare cases including: including breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) and other lymphomas, as well as squamous cell carcinoma.)
Resource:
Breast Cancer Risk Factors You Can’t Change | American Cancer Society
Lifestyle-related Breast Cancer Risk Factors | American Cancer Society
NFCR-Supported Researchers Working on Breast Cancer
Daniel A. Haber, M.D., Ph.D.
Massachusetts General Hospital Cancer Center
James P. Basilion, Ph.D.
Case Western Reserve University
Xiang-Lei Yang, Ph.D. and Paul Schimmel, Ph.D.
Scripps Research
Danny R. Welch, Ph.D.
University of Kansas Cancer Center
Ronald A. DePinho, M.D.
University of Texas MD Anderson Cancer Center
Susan Band Horwitz, Ph.D.
Albert Einstein College of Medicine
Amos B. Smith III, Ph.D.
University of Pennsylvania