Credentials
Massachusetts General Hospital Cancer Center
Boston, Massachusetts
Director, Massachusetts General Hospital Cancer Center
Professor of Oncology, Harvard Medical School
Research Projects
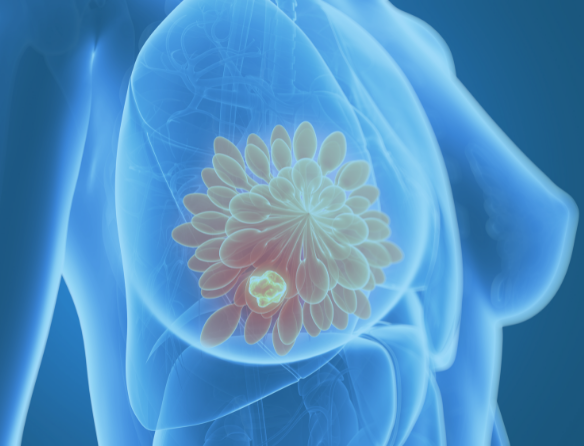
Dr. Haber is a renowned leader on genetic abnormalities of cancer – from inherited mutations (with familial predisposition) to mutations that are acquired by tumors themselves. With NFCR funding since 2000, his research aims to guide targeted drug therapies.
Focusing on circulating tumor cells (CTCs) that are shed from a primary tumor and metastatic sites and then enter the bloodstream, he and his collaborators developed the CTC-iChip—an advanced micro-engineered device that captures the few CTCs lurking between the millions of healthy cells in a standard blood sample from a patient.
Their research has developed methods to culture viable CTCs to increase their numbers, conduct genetic testing and other tests, which results can dramatically improve treatment and diagnosis for patients with many types of cancers.
The CTC-iChip is already used in some clinical research laboratories and will be submitted for FDA-approval. Oncologists can then use the blood test to obtain results to make timely life-saving treatment decisions for their patients.
In a new collaboration with NFCR-supported scientist Dr. Esther Rheinbay also at MGH, their research is confirming a target to develop a new treatment for the most deadly subtype of breast cancer, triple-negative breast cancer (TNBC). Overexpression or amplification of the Androgen Receptor (AR) occurs in 10% of TNBC. Unlike prostate cancer, AR expression abnormalities do not respond to anti-androgens. Dr. Haber’s team is obtaining sequencing and ‘omics data’ (DNA or genomic and RNA or transcriptome) from patients’ CTCs with and without AR abnormalities. Dr. Rheinbay’s lab analyzes the omic data to identify genes, transcription factors, and DNA regulators that contribute to the lack of response of anti-androgens. Their work may identify new targets that could lead to a treatment option and give patients with TNBC the hope they need.
Background
Daniel A. Haber, M.D., Ph.D., is the Director of the Massachusetts General Hospital (MGH) Cancer Center and a professor of oncology at Harvard Medical School. He received his Bachelor and Master degrees from the Massachusetts Institute of Technology (MIT), and received a M.D. and Ph.D. from Stanford University School of Medicine. Following his schooling, Dr. Haber conducted his postdoctoral training at MIT and joined the Harvard Medical School faculty in 1991 as an assistant professor.
Dr. Haber is most interested in the area of cancer genomics, including the study of circulating tumor cells, the Wilms tumor and genetic predisposition to breast cancer.
In addition to his award with NFCR, Dr. Haber is an elected member of the National Academy of Medicine, the National Academy of Science, a fellow of the American Academy of Arts and Sciences, on the Board of Directors for the American Association for Cancer Research and a member of the Association of American Physicians and the American Society for Clinical Investigation. He is also on the editorial boards of Cell, Cancer Cell, Molecular Cancer Research and Cancer Discovery and has served as genetics editor for the New England Journal of Medicine.
Dr. Haber has been honored with numerous awards such as the inaugural National Foundation for Cancer Research (NFCR) and the American Association for Cancer Research (AACR) Professorship in Basic Cancer Research, a MERIT Award from the National Cancer Institute, the Emil Freireich Award from MD Anderson Cancer Center, Stand Up to Cancer Dream Team Award, a Dream Team Award from the Prostate Cancer Foundation, the Sternlicht Award from Case Western Reserve and the Hinda Rosenthal Award for Translational Research from the AACR.

Our approach emphasizes a collaborative, team environment to accelerate new breakthroughs.