Free Cancer Screening Guidelines
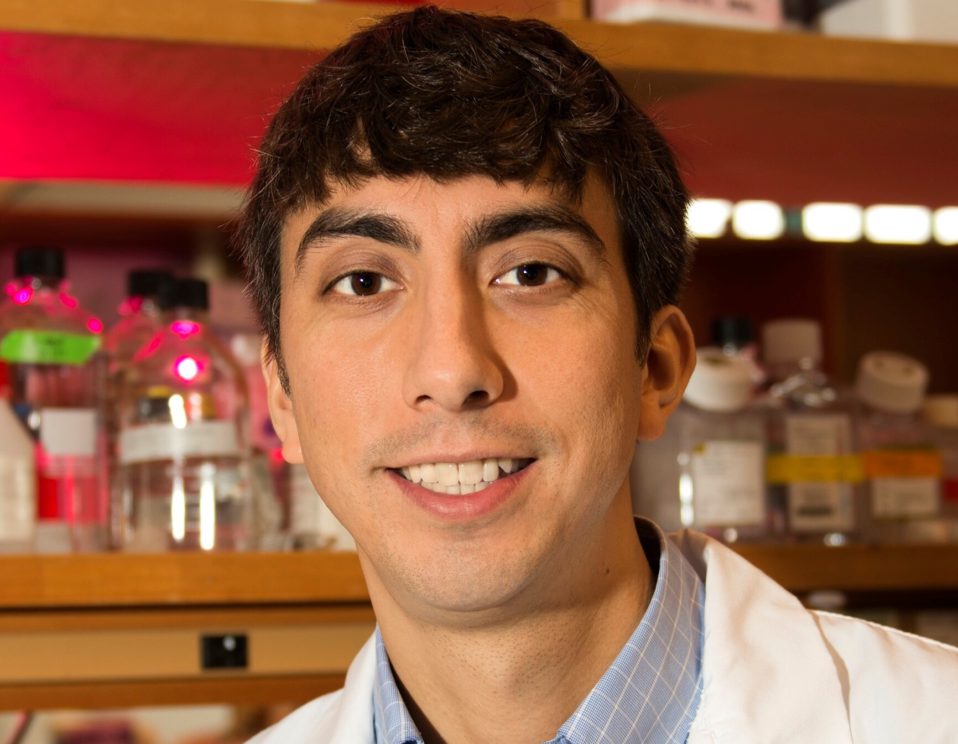
Scott Lippman, M.D.
Director, Moores Cancer Center, UC San Diego Health Scott M. Lippman, MD, is director of Moores Cancer Center at UC San Diego Health, professor of Medicine at UC San Diego School of Medicine, senior associate dean and associate vice chancellor for Cancer Research and Care and holds the Chugai Pharmaceutical…...
Dr. Karen Burke
Karen Burke is a Clinical Professor and research scientist in the Department of Dermatology at Mt. Sinai Medical Center (NY, NY) with a private practice in dermatology. After her Ph.D. in biophysics at Cornell University and post-doctoral research at Weill Cornell Medical College and The Rockefeller University, she completed her…...
Thea Tlsty, Ph.D.
Professor of Pathology & Director of the Center for Translational Research in the Molecular Genetics of Cancer, University of California San Francisco Director for the Program in Cell Cycling and Signaling, UCSF Helen Diller Family Comprehensive Cancer Center Dr. Thea Tlsty is Professor of Pathology at the University of California,…...
Susan Band Horwitz, Ph.D.
Distinguished Professor Emerita, Department of Molecular Pharmacology & Rose C. Falkenstein Chair in Cancer Research, Albert Einstein College of Medicine Dr. Horwitz is an American biochemist and distinguished professor emerita at the Albert Einstein College of Medicine. Dr. Horwitz grew up in Boston, went to Bryn Mawr College and received…...
William Werkmeister
Venture Capitalist and Partner Mr. William Werkmeister, also known as Bill, is a Founding Partner of the International Cancer Impact Fund, and in charge of the fund operations, organization, and capital raising efforts. He is a serial social venture capitalist and social entrepreneur. In addition to ICIF, Bill manages a…...
Robin Wang
Opera Singer, Angel Investor and Philanthropist Robin is a mezzo-soprano singer whose tone is described by the industry as “crystal-like” with the experience as in international singer. Her repertoire ranges from modern, classical, oriental and western styles. She has held concerts at the Kennedy Center, Lincoln Center, the United States,…...