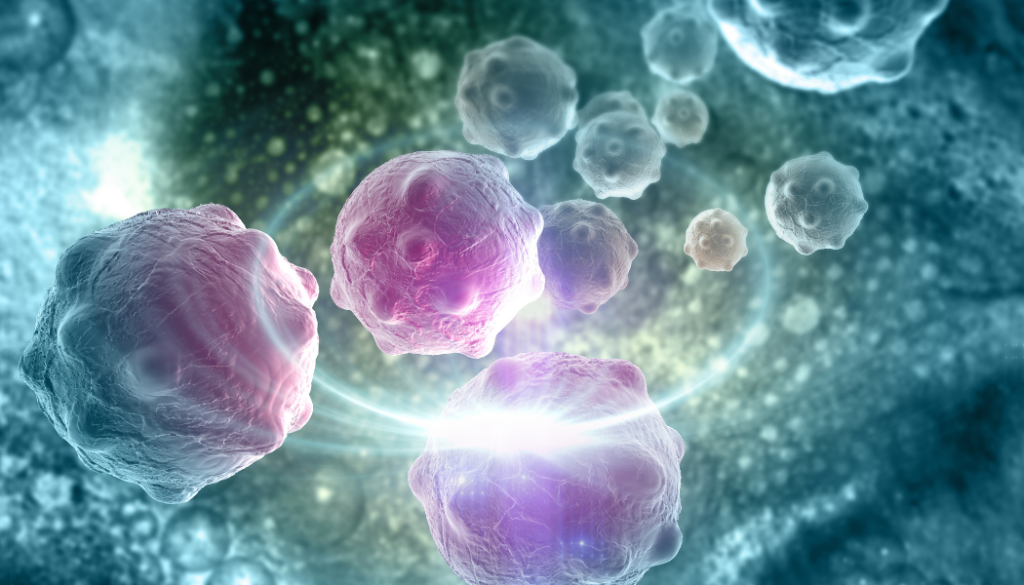
The prevalence of skin cancer is rising at an alarming rate, with melanoma being the deadliest. Melanoma is renowned for quickly spreading to other organs (or metastasizing), drastically decreasing the likelihood of survival. Being able to stop the spread of melanoma cells is essential to save the lives of many patients; however, no researcher has been able to solve the puzzle – until now. With long-term support from the National Foundation for Cancer Research (NFCR), Dr. Daniel Haber and his team developed the CTC-iChip – a medical device to capture the few circulating tumor cells (CTCs) present in a standard blood sample from a patient. Circulating tumor cells are tumor cells that have become detached from the primary tumor and enter the blood circulation. While CTCs occur once in a billion cells and are extremely rare, they nevertheless may hold the key to metastasis—the stage responsible for most cancer deaths. Dr. Haber and his team developed methods to analyze the genes in CTCs, providing a liquid biopsy and an invaluable window into a patient’s cancer in real-time. Doctors may efficiently obtain critical information from their patient’s CTCs for life-saving treatment decisions in advanced cancer with the liquid biopsy. Though this significant breakthrough sparked excitement throughout the oncology world, Dr. Haber continued digging for more pieces to the puzzle. He honed in on the unique makeup of CTCs to understand what fueled the spread of these deadly cells and what inhibited it. Using samples from melanoma patients, the team found that the unique lipogenesis regulator (referred to as SREBP2) held an important role in combating the growth of CTCs. SREBP2 directly induces transcription of the iron carrier, which kicks off a chain reaction at a cellular level. This chain reaction causes resistance to ferroptosis inducers, a type of programmed cell death. The ability to manufacture these chain reactions within CTCs opens up a realm of therapeutic opportunities for patients with metastatic melanoma. While this discovery is highly significant in the war on cancer, it is only just the beginning of understanding how to reduce melanoma metastasis. Dr. Haber remains committed to solving more pieces of the puzzle. To support the work of Dr. Haber and other world-renowned researchers, please make a gift today. Additional Reads You May Enjoy: New Drug Makes Unresectable or Metastatic Ocular Cancer Treatable Catching Cancer Cells on Their Way to Spreading Detecting Skin Cancer with Artificial Intelligence and Other Game-Changing Technologies in Cancer Stay connected with the cancer community! Receive NFCR’s monthly e-newsletter and blogs featuring stories of inspiration, support resources, cancer prevention tips, and more. Sign up here.