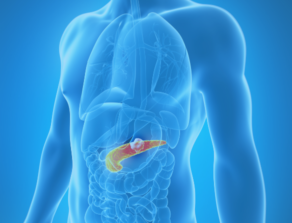
Pancreatic Cancer
Pancreatic cancer is the eighth and tenth most commonly diagnosed cancer in women and men, respectively, in the U.S. It is the fourth deadliest cancer for men and women. It is one of the few cancers for which survival has not improved substantially in over 40 years.
Key Facts
- An estimated 64,050 new cases of pancreatic cancer will be diagnosed in the U.S. in 2023, with 50,550 deaths expected to result from the diagnosis.
- Pancreatic cancer is expected to become the 2nd leading cause of cancer-related deaths in the U.S. by the year 2040.
- The overall five-year survival rate for pancreatic cancer is just 12%.
- Risk factors for developing pancreatic cancer include tobacco use, overweight and obesity, heavy alcohol consumption and exposure to certain chemicals, family history of the disease, age, chronic or hereditary pancreatitis, and long-standing type 2 diabetes. Individuals with Lynch syndrome and certain other genetic syndromes, as well as BRCA1 and BRCA2 mutation carriers, are also at increased risk.
Source: American Cancer Society’s Cancer Facts & Figures 2023 and American Society for Clinical Oncology (2020)
Signs and Symptoms
- Belly or back pain
- Jaundice – includes dark urine, light-colored stools, and itchy skin.
- Weight loss and poor appetite
- Nausea and vomiting
- Gallbladder or liver enlargement
- Fatigue
- Blood clots
- Diabetes
Source: American Cancer Society’s website 2023
64050
new cases expected in 2023 50550
deaths expected in 2023 12
% five-year survival rate
Pancreatic Cancer Awareness Month is recognized in November. To help accelerate cures please make a gift today.